How Does the Intrathecal Route Deliver Drugs?
Intrathecal drug delivery is a sophisticated method of administering medications directly into the spinal canal, offering distinct advantages for certain therapeutic contexts. The intrathecal route definition refers to the delivery of drugs into the cerebrospinal fluid (CSF), enabling direct interaction with the central nervous system (CNS). By bypassing conventional systemic pathways, this delivery route allows for targeted access to the CSF that surrounds the CNS. This approach provides higher concentrations of the drug at the target site while minimizing systemic side effects. Understanding the intricacies of this delivery method is crucial for healthcare professionals and researchers focused on neurological therapies. This article delves into the mechanisms of intrathecal drug delivery, explores its function within the human body, and examines the various applications and considerations relevant to clinical practice and drug development.
Understanding the Intrathecal Route of Drug Delivery
What Is Intrathecal Administration in Clinical Practice?
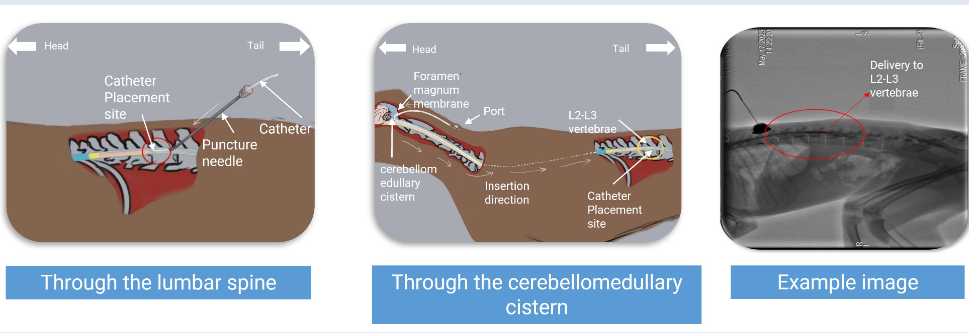
Intrathecal administration involves the injection of medication directly into the spinal canal, specifically into the CSF. Clinicians use this technique for several therapeutic purposes, primarily when treating chronic pain and spasticity that does not respond well to oral medications. One of the key advantages of this method is the ability to deliver drugs in lower doses, maximizing therapeutic effects while reducing toxicity risks. By understanding the pharmacokinetics of drugs administered intrathecally, clinicians can achieve optimal therapeutic outcomes. Real-world application often requires skilled practitioners to perform the procedure safely, emphasizing the need for specialized training and protocols.
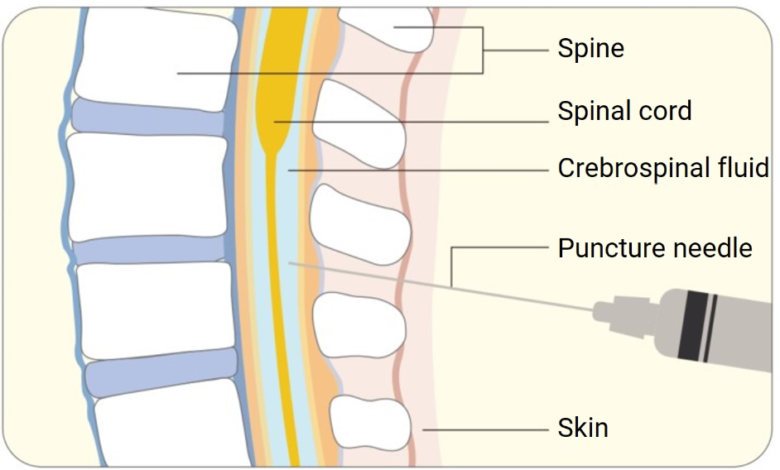
How the Spinal Canal Enables Direct Drug Transport
The spinal canal serves as a direct conduit for pharmaceutical compounds to reach the CNS. This structure’s unique access to the CSF ensures precise targeting of drugs, allowing faster onset of action when compared to oral or intravenous routes. Once injected, the medication disperses through the CSF, interacting with neural tissues rapidly. The natural flow of CSF facilitates the distribution of drugs, offering therapeutic relief effectively. By bypassing systemic circulation, intrathecal administration reduces side effects, achieving localized benefits, making it particularly beneficial for patients with CNS conditions requiring immediate intervention.
How Intrathecal Delivery Works in the Human Body
How Drugs Move in Cerebrospinal Fluid After Injection
Upon injection into the CSF, drugs distribute according to the dynamics of the fluid within the spinal canal. CSF, continuously produced and reabsorbed, circulates around the CNS, providing nutrients and removing waste, acting as a medium for drug dispersion. Medications administered intrathecally utilize this natural circulation to reach specific neural sites. The transport rate and distribution depend on the physicochemical properties of the drug, such as solubility and molecular weight. Understanding these properties allows for predictability in drug movement, enabling clinicians to dose effectively while foreseeing pharmacodynamic responses in patients.
How Intrathecal Delivery Bypasses the Blood–Brain Barrier
The blood-brain barrier (BBB) is a critical obstacle in CNS drug development, limiting the passage of therapeutic agents from systemic circulation into neural tissues. Intrathecal delivery circumvents this barrier by introducing medications directly into the CSF, facilitating immediate drug availability to the CNS. This bypass enables treatment of conditions like pain and severe spasticity, where conventional methods falter due to BBB constraints. Intrathecal delivery thus supports the administration of drugs that are too large or hydrophilic to cross the BBB. This precise targeting not only enhances efficacy but also offers an innovative pathway for developing CNS therapies.
See also: Emergency Ambulance and Its Role in Healthcare
Applications, Advantages, and Development Considerations
Key Therapeutic Areas Using Intrathecal Drug Delivery
Intrathecal drug delivery is particularly prevalent in managing chronic pain and spasticity. Conditions such as cancer-related pain, spinal cord injuries, and severe muscular disorders benefit significantly from this method. The ability to deliver high-concentration medications directly to affected areas allows for potent relief. Pain management, especially for non-responsive cases, leverages intrathecal pumps that deliver consistent dosages tailored for individual needs. By providing localized therapeutic effects, this approach improves patient outcomes, minimizes systemic exposure, and enhances quality of life for those dealing with debilitating CNS conditions.
Intrathecal Administration in CNS Drug Development Services
Intrathecal delivery offers substantial promise in advancing CNS drug development, creating avenues for novel therapeutics. Research and development services focus on leveraging this route to explore new formulations that address unmet medical needs. Drug manufacturers and researchers collaborate to optimize dosing strategies, ensuring safe and effective delivery. Intrathecal pathways are particularly attractive for conditions where the BBB limits traditional treatment options. With ongoing advancements in biotechnology, this delivery method continues to evolve, promising innovative solutions for complex neurological disorders that are otherwise challenging to treat.
Conclusion
Intrathecal drug delivery represents a breakthrough in CNS treatment, offering a direct approach to managing complex neurological conditions. Its ability to bypass the blood-brain barrier provides substantial therapeutic advantages, making it invaluable for pain management and spasticity. As drug development continues to evolve, intrathecal routes offer promising prospects for creating more effective CNS therapies. Healthcare professionals must remain informed about this technique’s capabilities, ensuring optimal patient care. Enhancing understanding and application ultimately supports improved therapeutic outcomes, paving the way for future innovations in CNS disease management.



